Definition of the problem
High infant mortality rate (IMR) – 14.9%o in 1999
IMR (a health outcome) has been selected as one of the priority problems in the Republic of Macedonia. The infant mortality rate was very high (over 100%o) in the 1960s, the "rapid" decline in the next two decades, reaching the value of 31.6%o in 1990. Even though the decreasing trend continued in the 1990s, IMR is still very high compared with other European countries and with other countries in the Region (Bulgaria 14.4%o, Greece 6.4%o, Croatia 8.2%o, Slovenia 5.2%o, Poland 12.2%o, Hungary 9.7%o Denmark 5.5%o, Sweden 3.8%o, Finland 3.9%o, Germany 4.9%o - WHO data base 1996/98)
The structure of infant deaths is as follows:
There is strong evidence that spending on the education of women and the quality of health care is cost-effective in reducing the IMR.
Ethical underpinnings of the problem
The general ethical orientation of the Macedonian society towards health is based on the principles of an egalitarian liberalism (every person has the right to health) and objective utilitarianism (good health is social good) and is regulated by the Constitution and the Health Insurance Law.
The basic determination in the Articles of the Constitution of the Republic of Macedonia is that the Republic of Macedonia is, among other facts, a social state. Article 34 of the Constitution defines another constitutional determination that citizens of the Republic of Macedonia have the right to social security and social insurance determined by, and it states that every citizen of the Republic of Macedonia has a guaranteed right to health protection and that the citizens of the Republic of Macedonia have the right and duty to protect and improve their own and health of others.
Accepting the Egalitarian liberalism approach, in a just and fair society the State has the responsibility to provide a certain minimum level of opportunity and resources for health care for all.
Objective utilitarianism evaluates consequences by looking at the well-being of all individuals in the society. Considering a health as a social good the state has the responsibility to mobilize funds for health services that can improve health, human capital and economic productivity of a nation.
Healthy children are the future of the nation.
Cause - diagnosis
Broad causes
During the diagnostic tree analysis we have found several broad causes for this health care problem, which are parts of different sectors of the society and should be analyzed and treated separately. Those broad causes are:
Analysis of broad causes
All these causes have significant impact on the infant mortality rate but we will focus our attention on the last one but not the least: inadequate health care (antenatal, delivery, perinatal and postneonatal) which can be directly affected by interventions in the health care system.
Inadequate health care is result of the insufficient quantity of services and low quality of health care.
1. Insufficient quantity of services is not result of the lack of access to the health care facilities, because whole territory of Macedonia is covered with health facilities (PHC and hospital) and all antenatal, delivery, perinatal and postneonatal services are completely covered with the Preventive Program for active mother and child health care, and are free of charge for all. According to this Program each pregnant woman should visit her oby&gyn specialist for first examination when the mother book is open for her and she is advised to have the antenatal services recommended in the mother book.
The evidence shows that the quantity of the services provided in the PHC departments for women and children are lower than recommended in the Program, and the reason for that is lack of knowledge for the need to use the health services due to lack of information and lack of health promotion activities for the pregnant women and mothers, especially in some rural and poor urban communities, where they are combined with other factors such as environmental conditions for health, socioeconomic status, poverty, education, culture, religion, tradition, behavior and lifestyle.
2. Low quality of services
Low quality of services is evident in both clinical and service quality caused by human recourses, organization and non-human recourses.
Linked problems and causes
2. Organization causes low clinical and service quality because of the following:
Problems
The analysis of the causes shows that most of them are result of the following problems:
Option development
1. FINANCING
Introduction
As presented in the table below the GDP per capita has been decreased in the period 1991-1997 while the rate of the registered unemployment has been continuously increasing reaching the value of 41.7% in 1997. This has had significant impact on the health financing sources, health needs and costs for the delivery of the health services.
Table 1- Macroeconomic indicators within the period 1991 - 1997
|
Indicators |
1991 |
1992 |
1993 |
1994 |
1995 |
1996 |
1997 |
|
GDP growth rate, % change |
-12.1 |
-21.1 |
-8.4 |
-4.0 |
-1.4 |
1.1 |
2.0 |
|
Annual inflation rate % |
- |
1690.7 |
349.8 |
118.9 |
15.9 |
4.2 |
4.4 |
|
GDP per capita, US$ |
2060 |
1832 |
1659 |
1616 |
1583 |
1581 |
1593 |
|
GDP PPP $ per capita |
- |
- |
- |
3965 |
4405 |
- |
- |
|
Government expenditure, % GDP |
- |
48.2 |
54.5 |
54.2 |
46.5 |
44.3 |
39.7 |
|
Health expenditure as % of GDP per capita |
4.8 |
5.5 |
4.8 |
4.6 |
5.0 |
- |
- |
|
Registered unemployment rate, % |
26.0 |
27.8 |
29.3 |
32.0 |
35.6 |
38.8 |
41.7 |
Source: Health for All database
In 1995 GDP per capita in PPP (purchasing power parity was) 4405US$. The same year GNP per capita was 1690 current US$ (without purchasing power parity adjustment).
Health expenditure per capita in PPPUS$ was 314 in 1995 (most recent year in the World Development indicators data base). In 1997 public health expenditure as a %GDP was 8%, while private health expenditure 1% in 1995 (only year data available in this data base).
The structure of the health care expenditure shows that 98% is in the public sector. Out-patient and in-patient care participate similarly with 39.4% and 39.3%.
Table 2 - State health care costs per categories, (%) of State health care costs
|
Costs |
1991 |
1992 |
1993 |
1994 |
1995 |
1996 |
1997 |
|
Out-patient health care |
31.2 |
43.0 |
46.5 |
45.5 |
43.0 |
40.9 |
39.4 |
|
Hospital care (including in-patient prescribing) |
43.3 |
35.8 |
35.6 |
36.9 |
36.6 |
32.8 |
39.3 |
|
Dental care |
3.4 |
3.5 |
4.2 |
4.5 |
5.4 |
5.0 |
5.6 |
|
Positive list drugs in state pharmacies |
15.8 |
15.7 |
10.0 |
8.9 |
10.0 |
10.7 |
10.3 |
|
Other health care costs |
3.9 |
0.3 |
0.3 |
0.2 |
1.5 |
0.7 |
0.4 |
|
Treatment abroad |
0.3 |
0.2 |
0.9 |
1.1 |
1.8 |
1.9 |
2.2 |
|
Investments and capital projects |
- |
0.7 |
1.6 |
2.5 |
0.2 |
1.1 |
0.7 |
|
Vertical program expenditures |
2.1 |
0.8 |
0.9 |
0.4 |
1.5 |
3.1 |
2.1 |
Source Health Insurance Fund, 1998
The sources of the health care financing are social health insurance, general revenues, self-payment and others. (Presented in the table below and in the scheme 2)
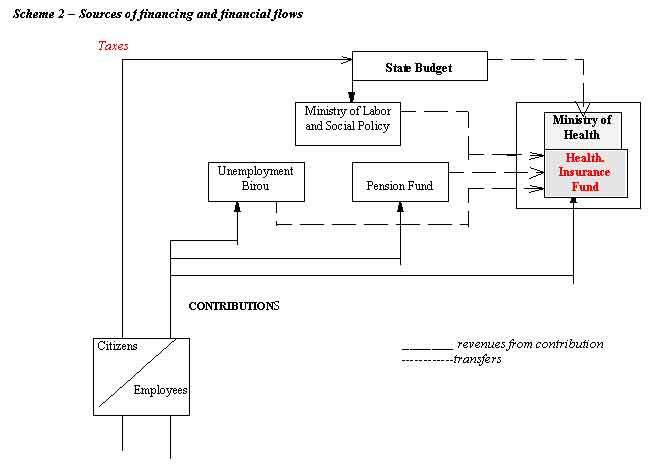
Table 3 - Main sources of health care financing (%) in
Republic of Macedonia 1991–1999
|
Sources |
1991 |
1992 |
1993 |
1994 |
1995 |
1996 |
1997 |
1998 |
1999 |
|
Health Insurance Fund |
82.2 |
79.1 |
82.3 |
79.5 |
78.8 |
80.1 |
82.9 |
80.1 |
79.1 |
|
State Budget |
- |
- |
- |
2.5 |
3.1 |
3.5 |
2.2 |
2.9 |
2.3 |
|
Self - payment (co-insurance and out of pocket) |
14.6 |
18.4 |
15.1 |
14.0 |
23.1 |
14.5 |
13.0 |
10.4 |
11.6 |
|
Other sources |
3.2 |
2.5 |
2.6 |
4.0 |
4.1 |
1.9 |
1.9 |
6.6 |
7.0 |
Source: Health Insurance Fund. 2000
Compulsory social health insurance is the main source for the health care financing participating with 79.1% in 1999. The general revenue i.e. State budget participates with only 2.3% in the total health financing. Self-payment participates with 11.6% and other sources (from sale, subsidies, rents, donations, grants) with 7.0%.
1. Compulsory social health insurance
According to the principle of universality, insurance is compulsory for all citizens of the Republic of Macedonia. Those employed in public and private enterprises and other employers (8.6% payroll of the gross salary), pensioners (counted as 14.694% of the net pension reimbursement), farmers (15% of the catastar income or 2.8% of the lowest gross price per family member but in total not more than 8.6% of the gross lowest labor price for all family members). For the unemployed persons, social cases, war veterans, disabled the rate is 12.465% of the basis i.e.70% of the lowest net salary announced by the Ministry of labor and Social welfare. These contribution rates are defined and issued by the Parliament. The Law proposes additional compulsory insurance in case of injury at work or professional illness, and the rate of this additional contribution is established at 0,5 % of the gross salary amount, i.e.1.8 of the legal entity’s profit.
In the Health Insurance Law the voluntary health insurance was stipulated and can be implemented only through private insurance companies. The benefits from the compulsory insurance are not allowed to be covered by the voluntary insurance.
Table 4 : Sources of Health Insurance Fund revenues in %
|
Sources |
1991 |
1992 |
1993 |
1994 |
1995 |
1996 |
1997 |
|
Revenues from previous year |
0.3 |
- |
- |
- |
1.2 |
- |
3.4 |
|
Personal contributions |
79.4 |
75.1 |
79.3 |
73.8 |
68.8 |
64.8 |
62.9 |
|
Transfers from Fund for Pension and Disability Insurance |
15.8 |
17.9 |
18.4 |
22.8 |
25.0 |
21.7 |
22.8 |
|
Transfers from Employment Bureau |
0.5 |
0.6 |
0.4 |
2.3 |
2.3 |
7.5 |
8.4 |
|
Transfers from Ministry of Labor and Social Welfare |
0.9 |
0.2 |
0.3 |
0.4 |
0.5 |
0.4 |
0.4 |
|
Transfers from the State budget |
0.7 |
4.9 |
0.8 |
- |
1.6 |
1.9 |
1.3 |
|
Other revenues |
2.4 |
1.3 |
0.8 |
0.7 |
0.6 |
3.7 |
0.8 |
Source: Health Insurance Fund, 2000
The structure of the Health Insurance Fund revenues shows that dominant source are the contributions of the insured (63%), than the Pension Fund is the second with participation of 20%, Employment Bureau contributes with 11% for the unemployed and the State budget for the same risk groups (age, sex, disease) who are not insurance and vertical preventive programs.
2. General revenues
The general revenues of the State budget are collected from these sources:
The funds allocated for health are very low and participate with only 0.5% in the total budget. There are nine preventive programs that should be fully covered by the state budget, but in reality the State budget participates with small amount as presented in the table below:
Table 5 : Vertical preventive programs for the year 2000 and estimated budget
|
Programmes |
in 000 US$ |
% to be paid from the State budget |
Participation in total State health budget |
|
Program for general check-ups for school children and students |
238 |
12.8 |
9.0 |
|
Program for blood donation, organization and promotion |
56 |
13.8 |
2.1 |
|
Preventive health care program |
538 |
11.8 |
20.3 |
|
Program for compulsory immunization |
295 |
8.6 |
11.1 |
|
Program for against brucelosis |
72 |
12.1 |
2.7 |
|
Preventive TBC program |
140 |
21.4 |
5.3 |
|
Preventive AIDS Program |
81 |
16.1 |
3.0 |
|
Program for active mother and child care |
180 |
11.0 |
6.8 |
|
Program for dialyses, transplantation drugs, citostatics, insulin, growth hormone |
1050 |
4.2 |
39.7 |
|
TOTAL |
2650 |
100.0 |
Source: Official Gassete of RM
The rest of the funds for the implementation of these programs through the public health care organizations are covered by the Health Insurance Fund.
Self-payment (co - insurance)
There are two sources of funds for the services and drugs paid directly to the health organizations:
*The previous Law established the participation rate at 20 % of the price for the out – patient services and the drugs of the primary health – care and 10 % of the total hospital expenses. A high number of participation exempts were established.
The new Law proposes a new participation policy - co-payment (fixed amount with ceiling of 20% of the average costs for the health services or drugs provided), which will give equal opportunities for all policy holders and will globally be more favorable to all policy holders. With this Law the visits to the selected primary care physician are free. The poor (social cases) and mentally ill are exempted from co-payment.
Another exempt is proposed, equal for all policy holders who have , during a calendar year, paid their participation for various services amounting of 70 % of the average salary paid in the Republic of Macedonia. In such a case, they are exempted from all participation to the end of the calendar year. In some cases, the amount paid will be even more favorable and will be determined with Fund’s Enactment
Interventions through this control knob
Lack of funds and bad allocation are among the main causes for the inadequate health care for the pregnant women and their babies. To solve this problem we are recommending these options for this control knob:
The Government has targeted these population groups for subsidy and should provide money for the implementation of this program, which is 6.8% of total State health budget money for preventive programs (out of which the state budget covers only 11.0%) and through the Program for immunization (compulsory immunization for infants).
With the changes in the legal status of the Health Insurance Fund, which is now autonomous legal entity, there is a risk that the Fund will not continue to cover the costs for this program or it can continue if it is part of the basic benefit package which should be redesigned. The preventive activities of this program are part of the routine services provided by the health care providers
The funds for this Program can’t be provided with tax increasing because the rate of unemployment is very high and the employed workers in the formal sector have enough financial burden.
The only possibility is to reallocate some funds from the other sectors: education and social welfare and to use this money through joint activities for health promotion for the girls and women from rural and poor urban area (which will have direct impact on the broad causes for the high infant mortality rate such as lack of the knowledge for the need to use the health care services).
To continue with the implementation of the Perinatal project financially supported by the World Bank loan. The total value of the funds allocated for this project is around 4 million US$ mostly for medical equipment, training (physicians, nurses and managers), database and computers for the neonatal departments.
The Government is obtaining funds for the civil works for Pediatric and O&G clinic in Skopje to enable the reorganization of the services and installation of the new equipment.
The UNICEF Baby Friendly Hospitals initiative has already covered 18 maternity wards and will continue.
WHO – support with technical expertise, training, health promotion, joint project with UNICEF for CME for community nurses.
Japan’s Government has granted medical equipment for the neonatal units in Medical Centers in Bitola and Shtip and there are some other activities in progress.
There are other international donors who are donating mostly medical equipment.
Intervention: Ministry of health to coordinate the activities of all international agencies.
Design new basic benefit package and introduce all the prenatal, perinatal and postneonatal activities.
The current basic benefit package provided for those who are covered by compulsory health insurance is comprehensive, as follows: periodic health checks, preventative health care including immunization; primary health care; emergency medical care in institution or at home; health care for pregnant women; dental treatment and disease prevention; out-patient specialist health care; in-patient specialist care, including hotel services and rehabilitation; drugs from the positive list; orthopedic devices as identified in national guidance; reimbursement of salary during sick leave or maternity leave.
Preventive services form an important part of the package, and there are a number of vertical programs for the primary prevention, identification and treatment of a variety of conditions. These are financed from the state budget through the Ministry of Health, and are presented in the table above.
The primary functions of the health organizations are financed by National Health Insurance Fund and for preventive
Activities from the State budget. According to its monthly revenues, the HIF makes an advanced financing to the health organizations (for salaries of doctors and other medical staff; material and capital expenditures) and also on behalf of the health organizations for medicines from positive list, hospital drugs, energy cost etc. The main payment mechanism for public doctors, is salary. The salary level vary according to the age, experience, responsibilities and skills of the doctors. Salary payment for public doctors do not contain incentives for efficiency and no incentives to over-treat. The private doctors contracted by HIF are paid with fee for services with monthly ceiling.
A) Introduce CAPITATION for the primary care doctors (public and private) contracted by the Health Insurance Fund.
The capitation will be weighted by age, sex and rural / remote area and will cover 70% of the PHC doctors’ income.
B) TARGET PERFORMANCE payment mechanism for preventive activities – if doctor and his team accomplish more than 90% of planned preventive activities in The Preventive program for mother and child (listed below) will receive the rest 30% of his income.
Antenatal health care
Delivery health care
Postpartal health care
Perinatal, neonatal and postneonatal activities
C) Introduce transitional global budget for the hospitals - simple payment for different service categories based on average costs (greater autonomy, increased accountability, improved efficiency)
3. REGULATION
A) To change the Health Care Law and to define precisely the activities and the type of services that should be provided in certain type of health organization and to precise rights of patients. To change the Health Care Law and to give delegation to the Doctors Chamber for the accreditation of the physicians.
B) New regulation for accreditation of the facilities.
There are by-law for the minimum conditions in the health care organizations regarding space, equipment and health personnel. There is a need to up-date these by-law in accordance with the EU standards.
C) New by-laws: for payment of the PHC doctors, hospitals and for basic benefit package.
D) Criteria for contracting public and private providers.
E) Accreditation of the doctors
The Chamber to issue regulations for licensing, accreditation and reaccredidation of doctors.
F) Audit and peer review
To change the Health Care Law and to make medical audit compulsory through strengthening the Inspection Department of the Ministry of Health with involvement of the experts of that field.
G) Introduce practical guidelines and protocols.
To customize practical clinical guidelines for the management of the most common problems – Medical School.
4. ORGANISATION
5. PERSUASION
Political analysis
To implement the options recommended above there is a need of political mapping and political analysis of all stakeholders. The stakeholders, their position and power are presented in the table below.
PLAYERS POSITION POWER TYPE
GOVERNMENT HIGH SUPPORT HIGH PUBLIC
MINISTRY OF HEALTH HIGH SUPPORT HIGH PUBLIC
MINISTRY OF FINANCE LOW SUPPORT HIGH PUBLIC
MINISTRY OF EDUCATION LOW SUPPORT HIGH PUBLIC
MINISTRY OF SOCIAL LOW SUPPORT HIGH PUBLIC
WELFARE AND LABOUR
HEALTH INSURANCE FUND HIGH SUPPORT HIGH PUBLIC
PATIENTS HIGH SUPPORT LOW
HEALTH ORGANISATIONS MEDIUM SUPPORT HIGH PUBLIC
MEDICAL SCHOOL MEDIUM SUPPORT HIGH PUBLIC
DOCTORS CHAMBER HIGH SUPPORT HIGH NGO
MEDICAL ASSOCIATION HIGH SUPPORT HIGH NGO
MAS MEDIA MEDIUM SUPPORT HIGH
INTERNATIONAL AGENCIES HIGH SUPPORT HIGH
NGOS HIGH SUPPORT LOW
Looking at this table the impression is that more or less all stakeholders will support the recommended options. But if we do deeper political analysis we will see that there is a need for special strategy for each stakeholder.
The Government in general is highly supporting the general policy for special protection of the mothers and children (Constitution). The result of that policy is the Preventive Program for mother and child health care and the Government will make efforts within the Cabinet to find funds for full financial coverage of that Program. On the level of the Prime Minister cabinet there is a need the Minister of Health to have more active role especially to convince the Minister of finance to reallocate more funds for the Ministry of health for the Preventive program for mother and child.
The justification for reallocation of the funds from the other sectors is this: the Ministry of health, Ministry of education and Ministry of social welfare and labor to run together the Program for health information, promotion and education for girls and women especially those who are poor and in rural areas, using the available resources (teachers, health personnel, social workers). On that way some of the funds will be saved and can be directed for this Program instead of using more funds through the three Ministries for individual not coordinated Programs. That will enable to reallocate some funds for the Preventive program only for health services (preventive). Action: Minister of Health to negotiate with the Minister of finance, education and social welfare and labor. The Steering Committee to be established to coordinate and monitor all these activities on the level of Cabinet.
The Minister of Health to establish the Coordination Committee as an Advisory body for the implementation and evaluation of all interventions undertaken to improve the quality of the obstetric, perinatal and postnaeonatal health care. This body will be with representatives from: Medical Association, Doctors Chamber, Nursing Association, experts from the Medical School, Clinical center, secondary and primary health care organizations, HIF, journalist).
The Health Insurance Fund will be highly supportive because the recommended interventions are beneficial for the Fund:
1. With full Government financial coverage of the Preventive program for mother and child the Fund will save money and can reallocate some funds for the preventive services for the insured as per the Program.
2. With improvement of the contribution collection, increasing the efficiency and capacity building, information system, the Fund will increase the revenues and eventually decrease the unnecessary expenditures.
The directors of the health organizations have high power and will be medium supportive because will be given autonomy, but also financial accountability, and will have to improve the efficiency and quality of the health services using the protocols and standards.
Medical School and Nursing School will be supportive but probably there is a need of more resources for changing the curricula, CME and evidence based protocols and guidelines.
Medical Association and Nursing association will support the recommended interventions because the health doctors and nurses will benefit with the training, and financial incentives.
Doctor’s Chamber will be supportive because the Chamber will be authorized for the license, accreditation and reaccredidation of the doctors.
All mentioned professional associations will be supportive to these interventions because they will be directly involved in the implementation with their representatives in the Coordination Committee.
The patients when well informed for all activities will be supportive. At the moment there are not well organized and their power is low. There is a need of urgent persuasion activities through the mass media and public information campaigns.
The mass media has high power but their support should be changed from medium to high. The journalist from the Coordination Committee and the appointed official from the Ministry of health (PR officer) will be in charge to communicate with the media and to organize the public campaign.
International agencies like UNICEF and WHO will be high supportive and have high power. There is a need for coordination of the recommended activities with their activities.
Non-Government organizations have low power but can be supportive especially if their activities are in this field.